Classification
Classification of periodontal and peri-implant diseases and conditions (2017)
Key aspects of the new classification
The new classification of periodontal and peri-implant diseases and conditions, devised by mutual efforts of the AAP and the EFP, and introduced in 2017, brought several key updates:
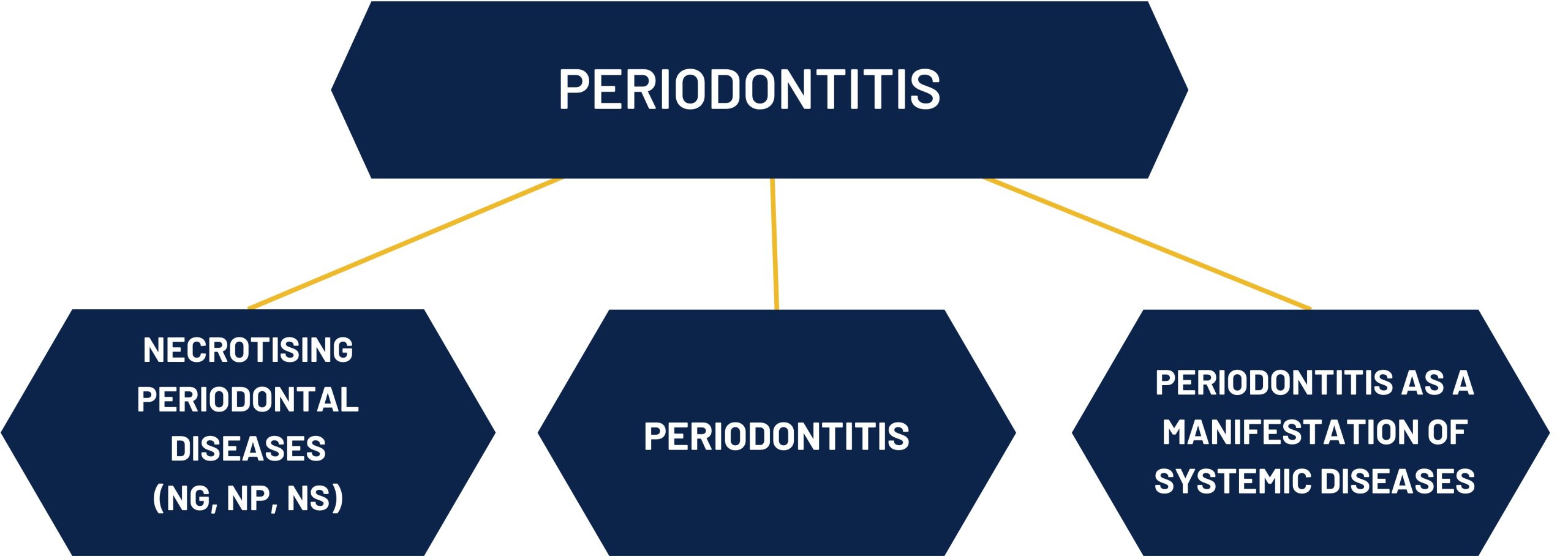
Periodontitis Classification: It includes a multi-dimensional STAGING and GRADING system, which enables assessment of the severity and complexity of the disease
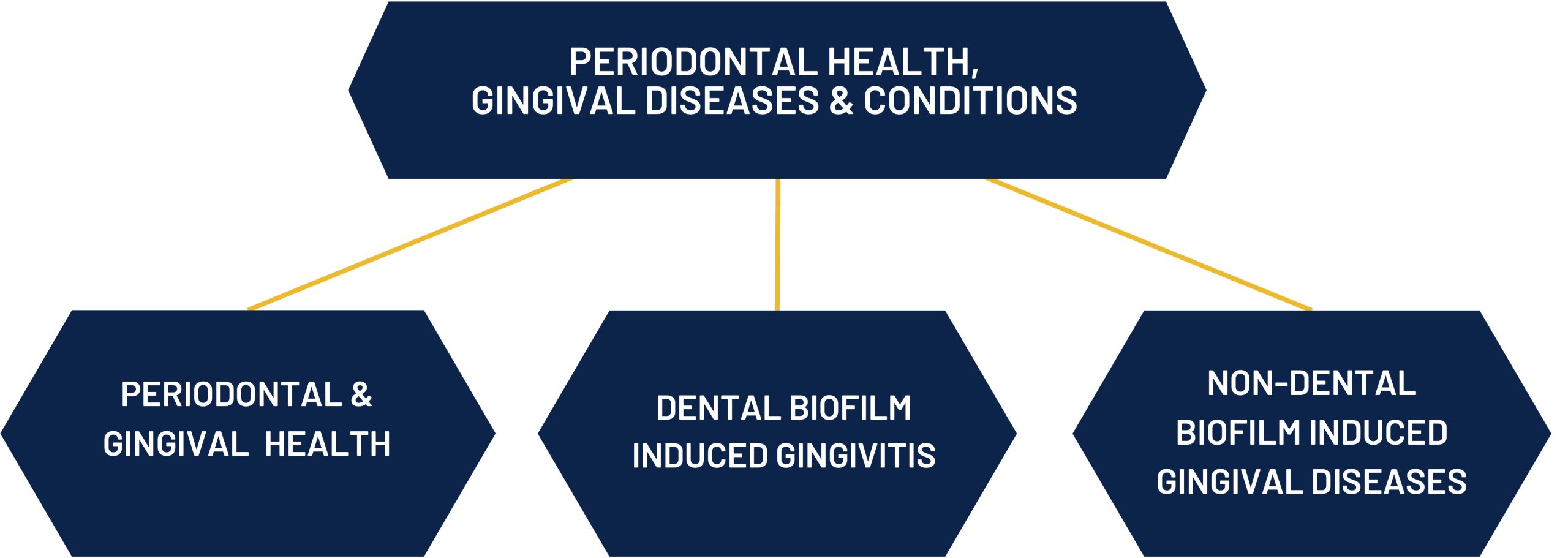
Periodontal Health and Gingival Diseases: This category provided definition of gingival and periodontal health and was expanded to include various forms of gingival diseases, both plaque-induced and non-plaque-induced.
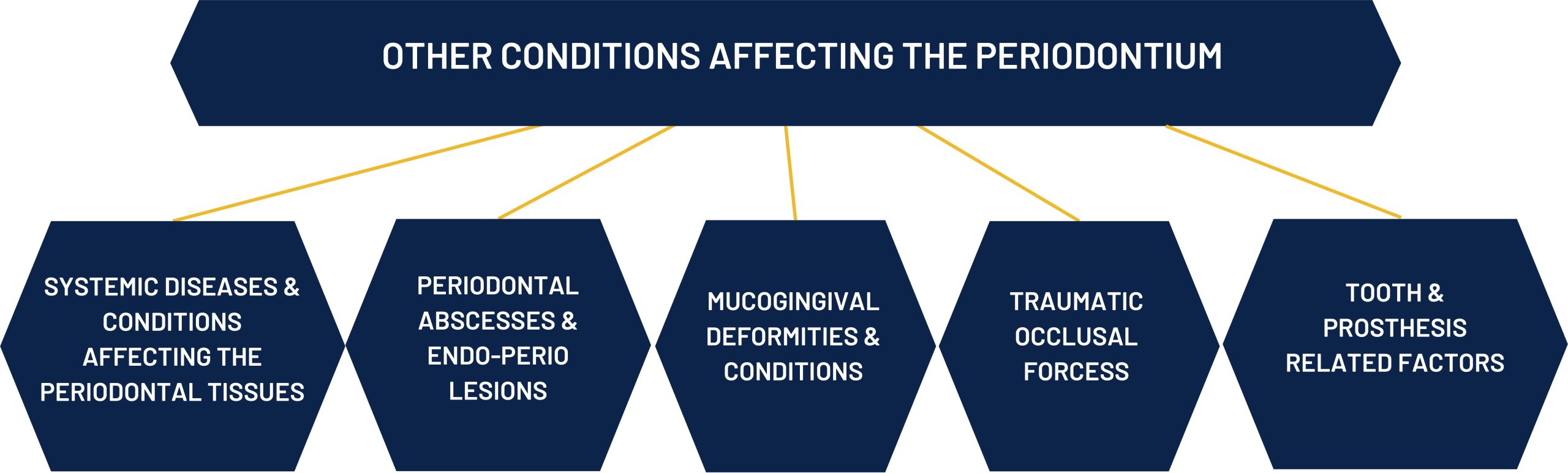
Other Conditions Affecting the Periodontium: This includes systemic diseases and conditions that affect periodontal health.
Peri-implant Diseases: For the first time, a classification for peri-implant diseases and conditions was introduced, recognising the importance of these conditions in modern dental practice.
These updates aim to provide a comprehensive framework for diagnosis and treatment, ensuring personalised patient care.
.
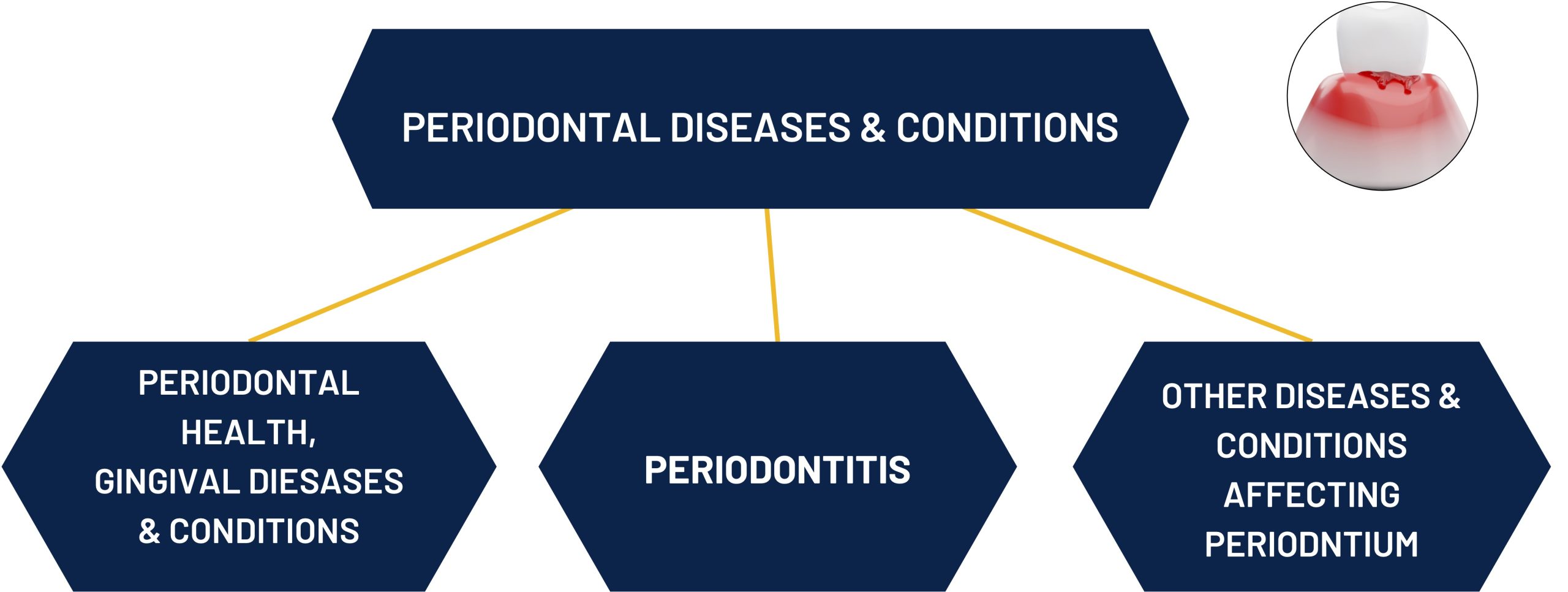
CLASSIFICATION OF PERIODONTAL DISEASES AND CONDITIONS
Caton, et al. 2018 link
CLASSIFICATION OF PERIODONTAL DISEASES AND CONDITIONS
CLASSIFICATION OF PERIODONTAL DISEASES AND CONDITIONS
CLASSIFICATION OF PERIODONTAL DISEASES AND CONDITIONS
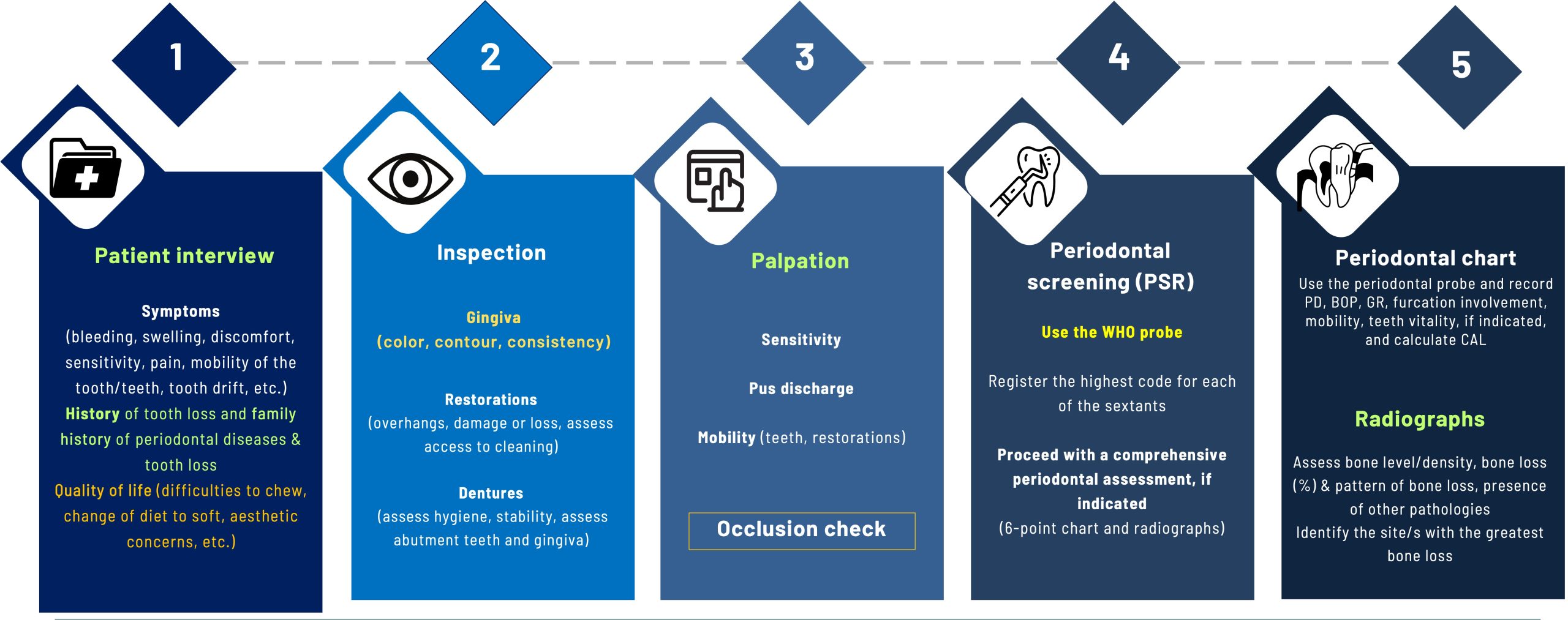
A structured periodontal assessment is essential for accurate diagnosis and effective patient care. The Basic Periodontal Assessment Flowchart provides a systematic approach to collecting key patient information beyond routine data. It captures details relevant to periodontal diagnosis and treatment, including specific symptoms (gingival bleeding, tooth mobility, and tooth drift), previous tooth loss and its causes, periodontal treatment history, and oral health-related quality of life.
By guiding clinical assessment and documenting essential findings, this flowchart may assist clinicians in evaluating patients’ disease status, tracking progression, and informing treatment planning.
Calibrated recording of key periodontal parameters—such as probing depths, bleeding on probing, clinical attachment loss, attachment loss in furcations, and tooth mobility, in addition to biofilm levels—ensures diagnostic consistency and enhances communication among dental professionals (links to diagnostics, periodontal chart, and API/SBI). Whether for initial screening or ongoing maintenance, a well-documented periodontal chart, combined with relevant radiographs (panoramic or full-mouth PA series), supports evidence-based decision-making and streamlines treatment planning.
BASIC PERIODONTAL ASSESSMENT FLOWCHART
Screening of patients
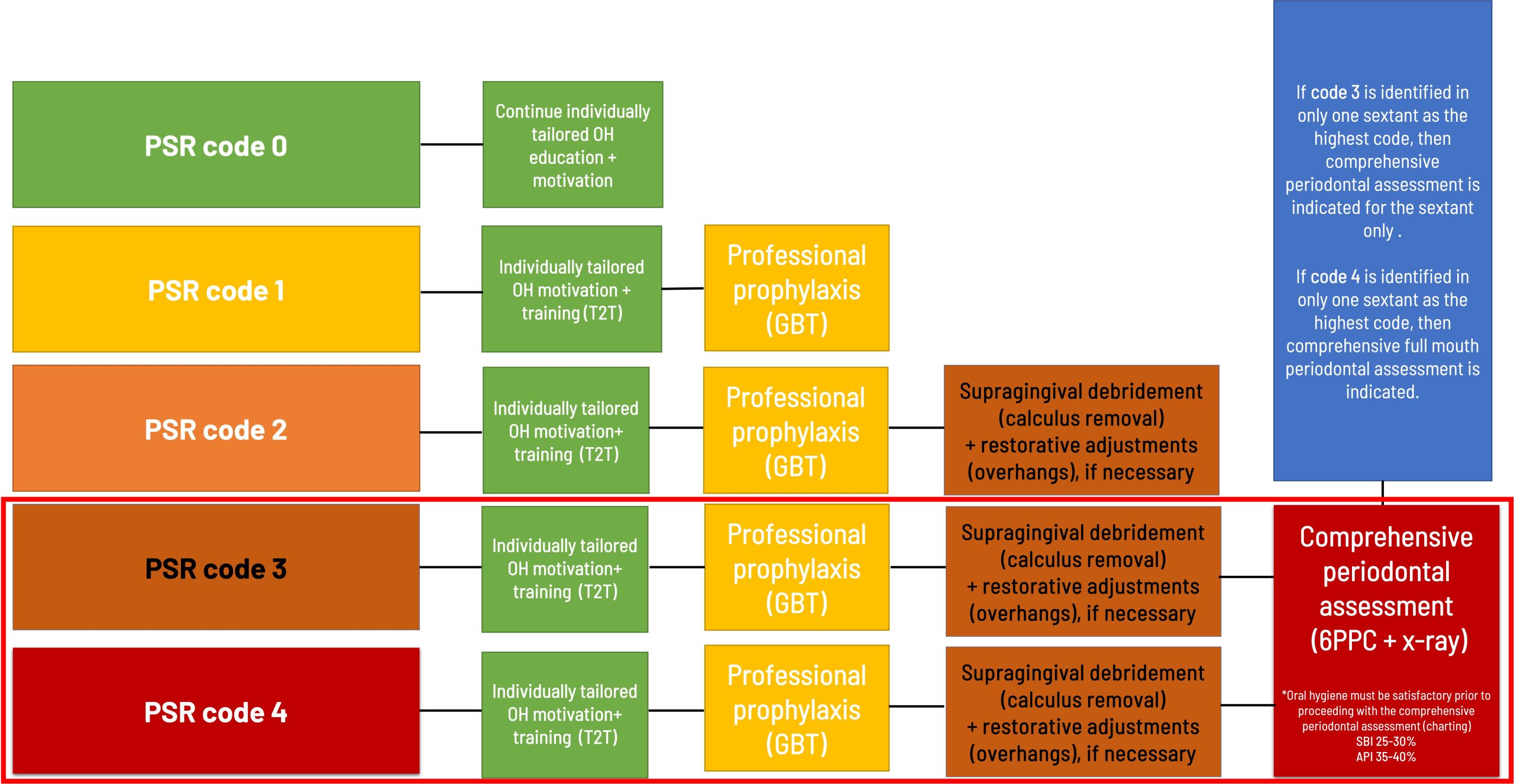
Each patient should be screened for the two most common oral diseases: caries and periodontitis. Based on the screening findings, further diagnostic steps should be undertaken if necessary. The Periodontal Screening and Recording (PSR) tool is used to differentiate between gingivitis and periodontitis. Patients suspected of having periodontitis must undergo a comprehensive periodontal and radiographic assessment to establish an accurate periodontal diagnosis
SCREENING TOOL FOR PERIODONTAL DISEASES
Following steps according to PSR results
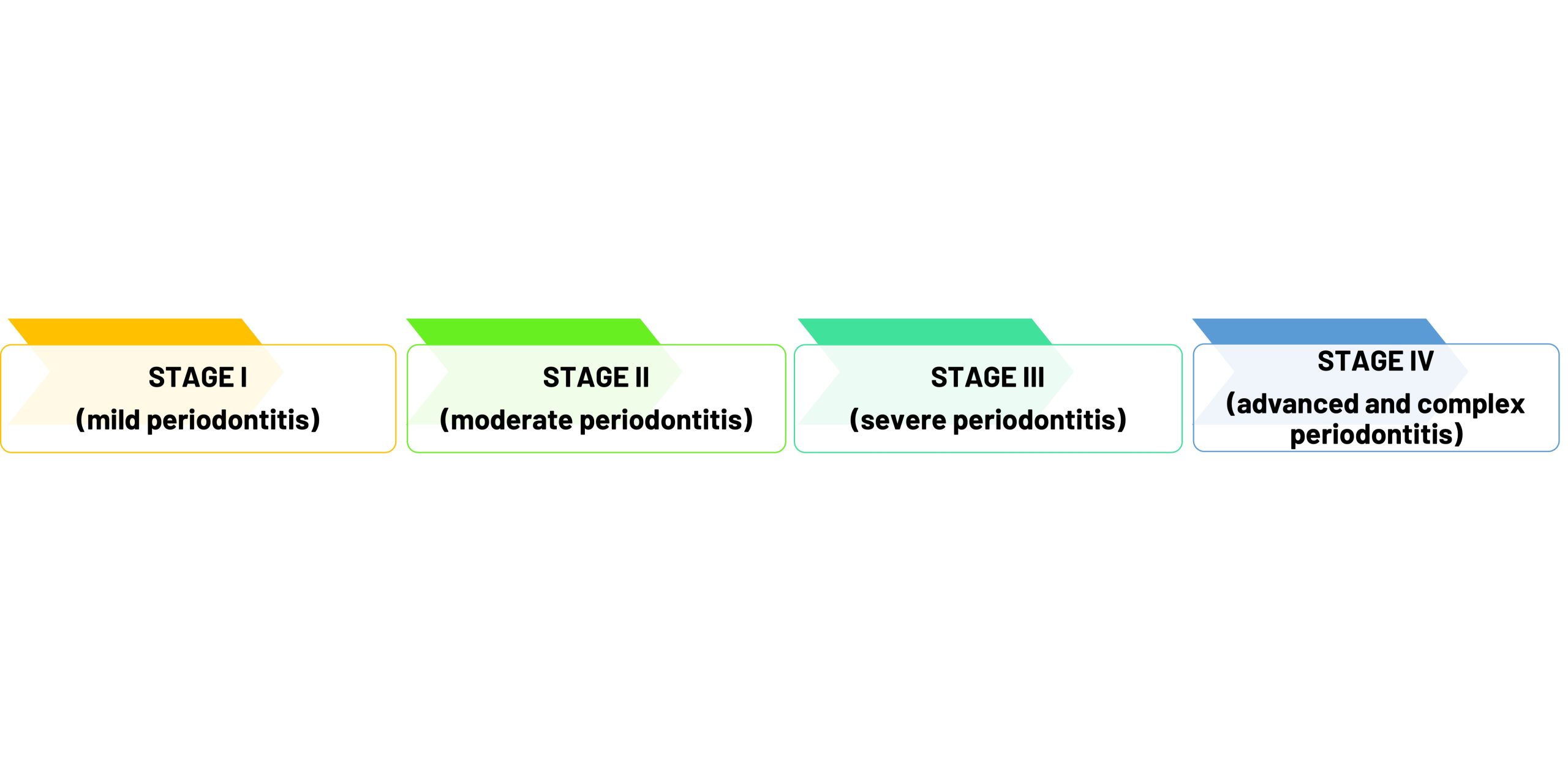
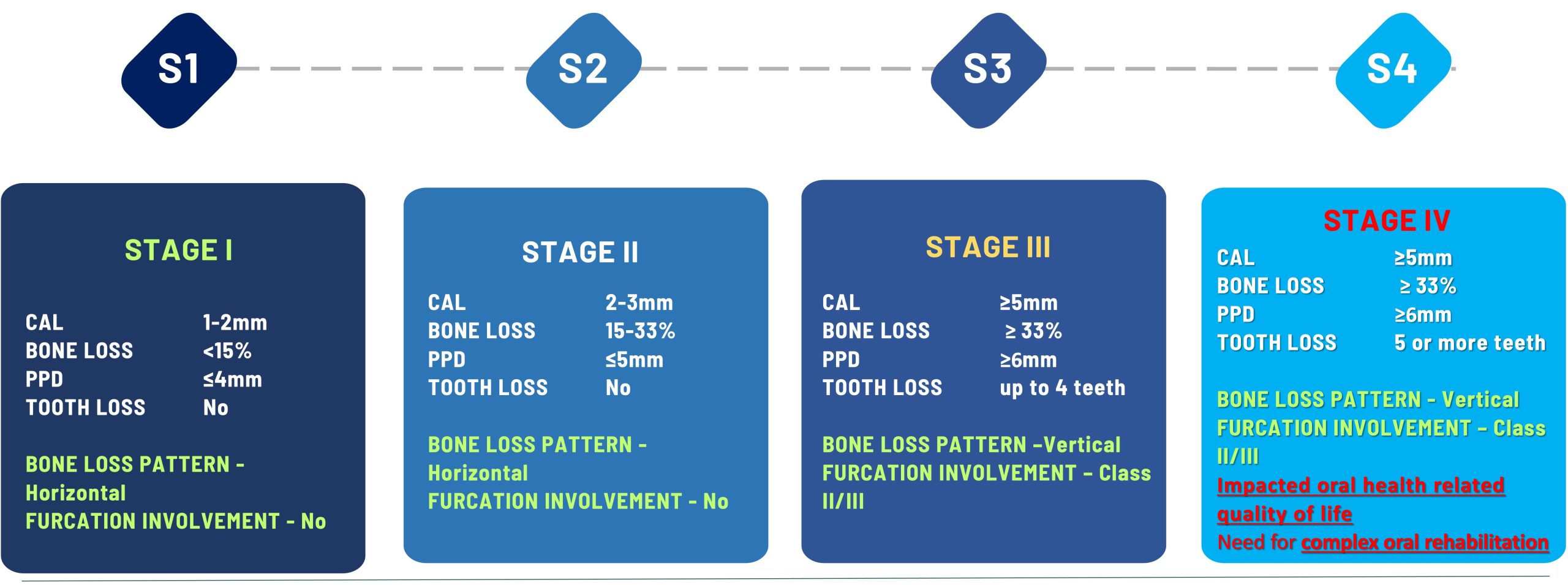
STAGING IN PERIODONTITIS
Staging periodontitis involves assessing the severity of the disease and the extent of damage to the supporting tissues and bone around the teeth.
Accurate staging requires a comprehensive evaluation of the patient’s history, along with detailed clinical and radiographic findings.
CLINICAL TIP FOR STAGING
It is always prudent to have a chairside guide at hand when making a diagnosis. However, it is essential to thoroughly evaluate all available clinical information, including (but not limited to) the patient’s history, periodontal chart, and current radiographs. Once established, the STAGE of periodontitis can progress over time, particularly in untreated or poorly controlled cases. Therefore, early, personalised treatment and continuous maintenance are fundamental to controlling periodontitis.
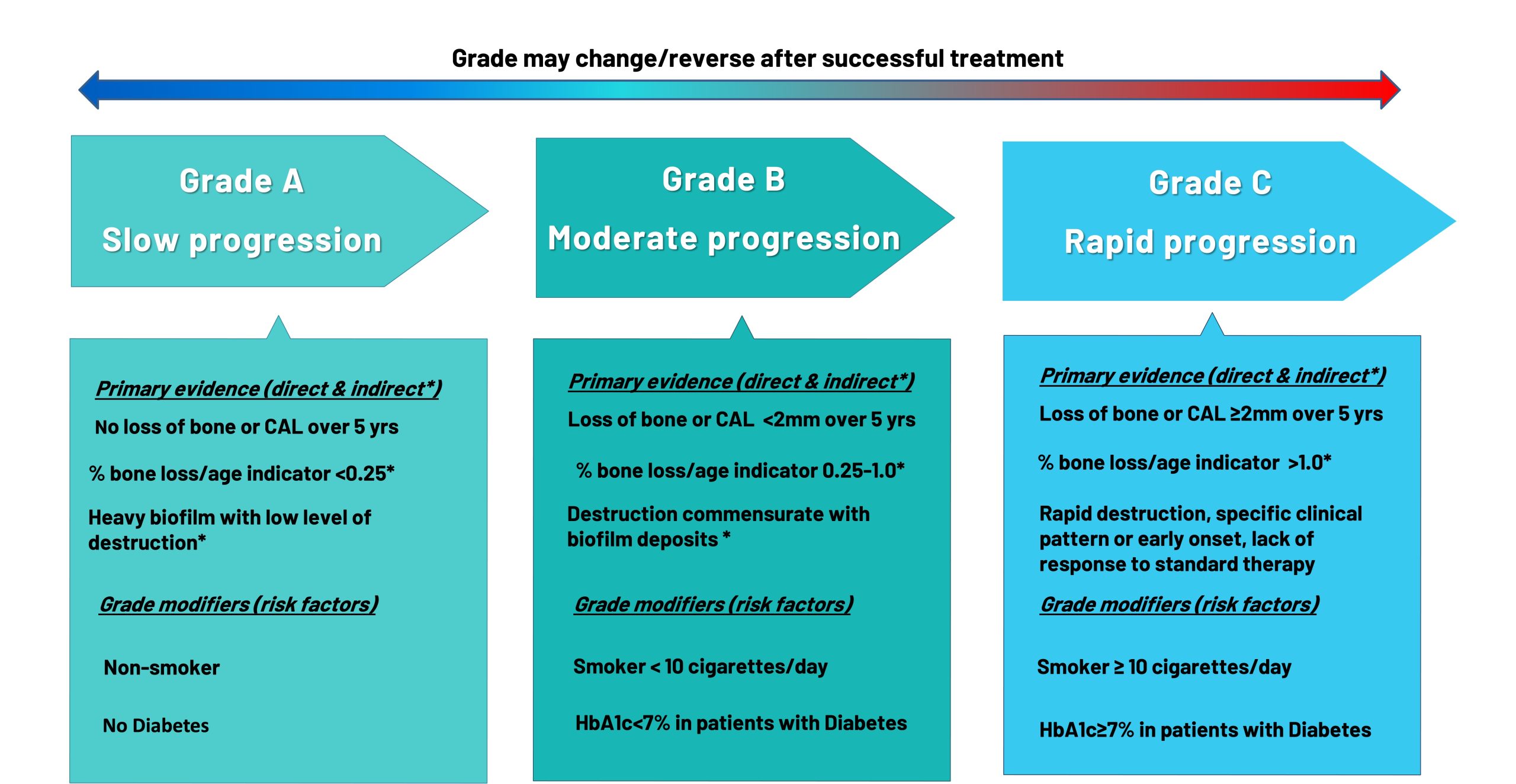
GRADING IN PERIODONTITIS
Grading is used to assess the rate of progression of periodontitis, the risk of further deterioration, and the impact of the disease on overall health.
It complements staging by adding a dynamic component to the diagnosis.
Grading helps personalise treatment strategies. Early identification of Grade C cases is critical to prevent further destruction.
Regular follow-ups and risk factor modification are essential for all grades.
CLINICAL TIP FOR GRADING
Which risk factors are currently used as denominators for grading?
Numerous risk factors may be linked with periodontitis, however diabetes and smoking are specifically emphasised in
grading because they have the strongest evidence for directly influencing the rate of disease progression and treatment outcomes.
Why not other risk factors?
Grading focuses on risk factors that are measurable, clinically relevant, and strongly tied to disease progression.
Factors like stress, genetic predisposition, or systemic diseases (e.g., osteoporosis) are important for understanding periodontitis but:
They are not measurable in a clinical setting.
Evidence linking them to the rate of disease progression is not as strong as for smoking and diabetes.
Including too many factors could complicate the grading process and make it less standardised.
Once a risk factor associated with a higher grade is identified, the patient’s overall grade may shift upward accordingly.
.
References:
Heitz-Mayfield LJA. Conventional diagnostic criteria for periodontal diseases (plaque-induced gingivitis and periodontitis). Periodontol 2000. 2024 Jun;95(1):10-19. doi: 10.1111/prd.12579. Epub 2024 Jun 3. PMID: 38831568